How To Pack Your Diabetes Emergency Kit
Preparing for an emergency is essential, particularly if you have a chronic health condition like diabetes.
Putting together a diabetic emergency kit can be reassuring and helpful, making you feel safer while traveling or going about your daily activities. However, knowing what to include in your kit may initially feel confusing.
You can purchase premade diabetic emergency kits, but it is often preferable to assemble your own. This allows you to tailor it to your specific requirements. Generally, it would help if you had sufficient diabetic supplies in your kit to last at least one week.
We will break down common and recommended supplies to assist you in assembling your emergency kit for diabetics.
Supplies to include
Your kit’s contents will vary based on the type of diabetes you have and your requirements. Before discussing diabetes-specific medical supplies, let’s review the necessary identification and medical information.
In an emergency, bystanders should be able to identify your name and contact information.
In a worst-case scenario, first responders must be aware of your medications and other health conditions that may affect your care.
Include the following in a sealed (waterproof) plastic bag with your medical information:
- A list of any other medical conditions you may have
- Any medication allergies
- Copies of your prescriptions with up-to-date dosages
- Basal rates, insulin-to-carb ratio, blood sugar target, insulin sensitivity factor, and correction factors for your insulin pump
- Names and phone numbers for your pharmacy and doctor’s offices
- An emergency contact’s information
- Make, model, and a serial number of your insulin pump or glucose monitor.
- Copy of your photo ID and health insurance card
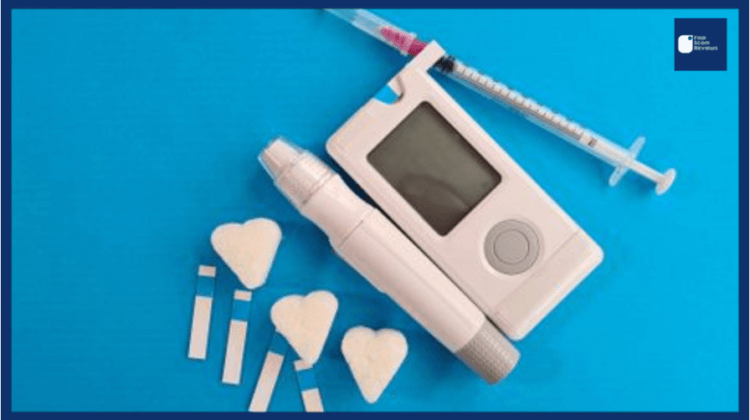
You should pack enough supplies for at least one to two weeks. The Centers for Disease Control and Prevention (CDC) and the Diabetes Disaster Response Coalition recommend the inclusion of the following items:
- Insulin and syringes for each injection
- Glucose meter
- Extra batteries for the glucose meter and insulin pump
- Lancets and lancing devices
- Insulin pump supplies, including additional pump sets and insertion devices
- Glucagon kits
- Alcohol wipes
- Glucose tablets (you can also pack quick carbs like honey, juice, or hard candy)
- Oral diabetes medication
- Empty plastic bottle or sharps container
- Water
Everything should be stored according to the manufacturer’s instructions. Check your emergency kit frequently to keep track of expiration dates and replace outdated items.
Do I require multiple kits?

While one comprehensive, well-stocked kit is sufficient for many individuals, some may feel more at ease with two large and one small kit. Others may prepare multiple kits for separate locations, such as their car or workplace.
Consider what will make you the most comfortable, and plan accordingly.
Here is how to construct the most effective diabetes emergency kits for any circumstance.
1. The Basic Diabetes Emergency Kit
Emergencies happen. Stressful days can cause an individual to miss a meal or even forget insulin. While you should keep items for routine lows in your daily kit, desk drawer, or bag, the following items are essential for a diabetes emergency kit. The following items should be included in every kit.
- An easily identifiable bag
- A backup meter with strips and lances
- A small container with a lid for used sharps and strips
- Alcohol swaps
- A glucagon kit
- Glucose gel, tabs, or other easily consumable preportioned snacks like a box of raisins
- A small supply of medications
- Pump change supplies
- A bottle of water
- A piece of paper or ID card with your diagnosis, emergency content
Every kit should be inspected every three to six months to ensure that medications and supplies have not expired and batteries are fully charged.
2. The Grab-and-Go
This can also serve as your “grab-and-go” emergency kit for situations where you need to leave quickly and don’t have time to prepare many supplies. In addition to the items listed in the “Basic Emergency Kit,” your Grab and Go emergency kit should contain the following:
- A larger waterproof container or bag with a handle for your supplies
- A compartment or inner storage for cold packs to store insulin
- Keep these in your freezer ready to go (not shoved behind freezer-burned peas)
- Syringes
- Pen needles (if you use an insulin pen)
- Basic first aid supplies
- Small scissors, bandages, etc.
- Medical tape, scissors, adhesive remover (or baby oil)
- A flashlight
- Food and water to last 2-3 days
- To save space, pack things like protein bars and other compact but nutrient-dense foods that fit your dietary needs
- Extra batteries and a charging bank
3. The Big Deal Kit
If you live in an area prone to extreme weather events or natural disasters such as hurricanes, earthquakes, or blizzards, or if you are someone who likes to be highly prepared, your kit should include:
- A larger cooler
- Ketone testing products
- Comfortable, durable shoes and extra socks in case of evacuation
- A blanket
- An emergency radio
- A list of your doctors’ numbers and locations
How long does a kit last?

Numerous medical supplies will include an expiration date. These must be replaced if they are not used, and it may be helpful to set reminders to rotate them out. When assembling your kit, note the expiration dates and label each item.
You can use up supplies to prevent waste and replenish the kit if you do.
Insulin has two expiration dates: one for unopened packages and one for opened packages.
After opening, most types of insulin must be used within 28 to 30 days. If you refrigerate your insulin kit, it can remain unopened for several months. Be sure to read the storage instructions on the label of your prescription medication.
Depending on how they are stored, the shelf lives of multiple diabetic emergency kits will vary. For instance, a car kit containing insulin will need to be replaced more frequently than a refrigerated office kit.
If your emergency contact information, insurance policy, or medical records change, it is essential to update these components of your kit.
Temperature matters
Here are some critical guidelines for maximizing your diabetic emergency kit and preventing damage:
Aim for a temperature of room temperature or below.
If you cannot refrigerate your insulin, the CDC recommends storing it between 59 and 86 degrees Fahrenheit (15 and 30 degrees Celsius).
Avoid storing your equipment in direct sunlight or in a location where it could be damaged by water.
Insulin loses its effectiveness when frozen, so do not use frozen insulin (even after it has been thawed).
ALSO READ: Coptic Salt For Type 2 Diabetes: Critical Report Amazing 1 Answer
What is a diabetic emergency?
In addition to having a diabetic kit for natural disasters, power outages, and national security incidents, diabetes-related medical emergencies can occur.
Having all your supplies in a single location makes everything easier to manage, and you’ll have peace of mind knowing that your equipment is readily available if you need it.
Knowing the symptoms and causes of diabetic emergencies can help you be prepared. Educating your family, friends, and coworkers on how they can assist you in the event of a diabetic emergency can make everyone feel more prepared.
Immediately contact emergency medical services if you or a loved one is experiencing a diabetic emergency.
Hyperglycemic hyperosmolar syndrome (HHS)
Hyperglycemic hyperosmolar syndrome (HHS) is a potentially fatal condition that can occur when blood sugar levels become extremely high. The kidneys then attempt to alleviate this by eliminating some glucose via urine.
Possible symptoms include:
- Excessive thirst
- Frequent urination
- Fever or sweating
If you do not replace the fluids you lose, your blood sugar levels will rise, and your blood will become more concentrated. Hyperosmolarity is the condition that causes organs, including the brain, to lose water.
HHS can be caused by illnesses that cause dehydration or reduce insulin activity in diabetics. Mainly at risk are older adults with type 2 diabetes.
Diabetic ketoacidosis (DKA)
Diabetic ketoacidosis is a complication of type 1 diabetes and, to a lesser extent, type 2 diabetes (DKA). This occurs when the blood sugar level is extremely high, and the concentration of ketones (acidic substances) in the blood becomes dangerously high.
DKA occurs when there is insufficient insulin to process high blood sugar levels. It may be the first sign of undiagnosed type 1 diabetes for some individuals.
Among the characteristic symptoms of DKA are:
- Frequent urination
- Extreme thirst
- Belly pain
- Nausea
- Fatigue
- Fruity-smelling breath
Home urine tests can monitor your ketones to prevent or detect a DKA emergency. Treatment consists of replenishing the body’s fluids and stabilizing blood sugar levels with insulin.
Diabetic coma
A diabetic coma can occur when either blood sugar levels are too low (hypoglycemia) or too high (hyperglycemia) (hyperglycemia).
If blood sugar levels are too high, dehydration and loss of consciousness can occur because the brain requires glucose to function. There is typically sufficient time to prevent hyperglycemia or hypoglycemia from becoming severe enough to cause a diabetic coma.
Check your glucose levels if you develop symptoms of high or low blood sugar, including:
- Fatigue
- Feeling flushed
- Upset stomach
Seek help immediately for more severe symptoms like:
- Vomiting
- Confusion
- Weakness
To treat a diabetic coma, prompt hospitalization is required so that doctors can monitor your vital signs and stabilize your blood sugar. Patients frequently recover completely and must develop a revised diabetes treatment plan.
Untreated diabetic coma can result in brain damage or death if left untreated.
Low blood sugar events
In both types of diabetes, experiencing a drop in blood sugar (a “low blood sugar event”) is quite common. This typically refers to hypoglycemia episodes that are relatively mild and treatable at home.
Four out of five patients with type 1 diabetes and nearly half of those with type 2 diabetes experience low blood sugar at least once per month, according to a major 2016 study.
Insulin shock
Insulin shock refers to an overabundance of insulin in the bloodstream. Insulin shock causes hypoglycemia and its associated symptoms. It can occur both whiles awake and asleep.
The National Institutes of Health (NIH) list the following as possible symptoms:
- Dizziness
- Shaking
- Fatigue
- Headache
- Hunger
- Incoherence
Situations that may result in insulin shock include:
- Taking too much insulin by accident
- Missing one or more meals
- Doing too much exercise without changing carbohydrate intake
The short-term treatment for diabetes consists of consuming a glucose tablet or a quick-acting carbohydrate and testing your blood sugar for 15 minutes. In severe cases, glucagon can also be used. Seek medical attention if your blood sugar does not rise.
Insulin shock is highly treatable, and mild cases can be treated at home using diabetic supplies. Nonetheless, if untreated, insulin shock can result in:
- Loss of consciousness
- Seizure
- Diabetic coma
- Death
Getting help
Based on their diabetes type and medical history, each individual may require a different assortment of items in their diabetes kit.
In addition to assembling and maintaining your kit(s), consider speaking with your doctor about what to do in an emergency to feel more prepared.
Here are some helpful questions you can ask:
- Exist diabetic emergencies for which I am at a greater risk based on my type of diabetes and medical history?
- Do any additional medical conditions increase my risk of experiencing an emergency? How do I determine whether I can handle an emergency on my own or whether I need to call 911?
Symptoms of diabetic emergencies, such as DKA or insulin shock, can appear suddenly, and knowing what to do can be crucial.
Summary – How To Pack Your Diabetes Emergency Kit
While premade diabetic emergency kits are available, assembling your kit allows you to meet your specific needs in the event of an emergency.
Include the following in a comprehensive collection of your medical information and essential supplies:
- Insulin
- Glucose monitor
- Snacks
- Water
It is essential to be aware of expiration dates and regularly update your kit. Keep the kit refrigerated or at room temperature, and protect it from extreme heat, cold, and moisture.
Knowing you have everything you need in the event of a diabetic emergency, such as diabetic ketoacidosis or insulin shock, can empower you and reduce your stress. Familiarize yourself with the warning signs of common diabetic emergencies, and do not hesitate to seek medical help if you experience any of them.